Civil War Medicine
by Dr. Bonnie Brice Dorwart
Civil War Medicine
How and where were physicians caring for soldiers in the Civil War educated? What did Civil War physicians think caused illness? What treatments did they use and why? What hampered their efforts to treat disease? What were the medical legacies of the Civil War? These are the questions we need to address if we are to understand Civil War medicine.
We now know a great deal about the previously little written-about subject of ante-bellum medical education because several lectures delivered to medical students in the 1850s were discovered in 2003 at the College of Physicians of Philadelphia, the oldest honorary medical academy in the United States, established in 1787. Most of these lectures were delivered at the University Of Pennsylvania School Of Medicine, and coincidentally, were heard by the author’s great grandfather who earned the M.D. degree there in 1851. These lectures and those from other medical schools of the period survived because their students paid to publish the ones they deemed significant.
Medical schools that trained most of the surgeons serving in the Civil War (all doctors were called surgeons during the War) would have existed between 1840 and 1860. Only the Allopathic schools (in contrast to many sects coexisting at the time, such as Eclectic, Botanico-Medical, Homeopathic) are listed below. The 51 institutions located in northern and southern states, as well as one each in California and Washington, D.C., are shown in Tables 1 and 2. Many schools opened, but closed before 1861, and are therefore not listed. The reader is referred to Dr. Robert G. Slawson’s exhaustive research in 2002 on this topic that can be accessed through the National Museum of Civil War Medicine.[1]
Table 1 Medical schools in northern states 1840-1860, with year founded[2]
Table 2 Medical schools in southern states 1840-1860, with year founded[3]
Until the Flexner Report of 1910, requirements for admission to medical schools were rudimentary at best. Even the two prestigious schools in Philadelphia, the University of Pennsylvania (“Penn”) and Jefferson Medical College, required only “one year of college work, in which, however, conditions have been very freely allowed.” and “a high school education or its equivalent,” respectively.[4]
Four semesters during two years comprised their medical training. Lecture topics at Penn from 1849-1851 for example, included Theory and Practice of Medicine, Anatomy, Materia Medica and Pharmacy, Chemistry, Surgery, Obstetrics and the Diseases of Women and Children, and Institutes of Medicine.[5]
Students at Penn in the 1840s and 1850s were taught that science is based on experience and making a “judgment” as to the correct answer to a question or a problem.[6]
Laboratory experiments were not mentioned. There was no concept of controlled trials, although the English naval physician James Lind published one on scurvy in 1753, and there was no notion of evidence-based medicine. Pupils were not told about Pierre C.A. Louis, M.D., who published a study in 1835 comparing the outcomes of consecutive patients with pneumonia and other illnesses treated by blood-letting with those who were not. He showed that there was no difference in survival. The practice of bleeding patients was still taught in 1851. Furthermore, these students were still learning that a “life force” was needed to direct the functions of the body, despite proof by Friedrich Wöhler in 1828 that no such force was required.
The following excerpts from other Penn lectures give us further insight into the information with which the students were imbued by their faculty.
Professor Francis Bacon Wood acknowledges that “members of the medical profession are not all knowing, and should strive to expand knowledge: Do we profess to have secret depths which ordinary intellect cannot fathom? Do we claim certainty or universality of knowledge, or infallibility of judgment? Or rather, do we not profess openly that our science is yet imperfect?—that, though much has been learned, yet much still remains to be learned?—that though we can do much good, we cannot do all good? Do we not proclaim that we seek only for truth; that we are open to its reception from whatever source it may come; and that our greatest zeal is to enlarge the boundaries of our knowledge, and the extent of our capacity of usefulness?” Professor Wood also directed the students to prepare “for the fearful encounter with disease to follow.” Lectures would teach them “the most characteristic and most important points of each subject,” but students are directed to learn “minute details… [from] published treatises and private study.”[7]
Professor Samuel Jackson gave the future doctors a perspective of the profession: “The object you propose to yourselves in coming to this city is laudable; the motives that govern your selection of medicine as a profession are noble. You would be physicians—men-healers—men-savers. It is in the order of Providence that all that live must suffer and die. None are exempt from this universal law. …While suffering, disease, and death are knitted with the life yarn of man into his existence, yet is there much of each wholly avoidable… which may be prevented, and from which he may be saved.”[8]
Professor William E. Horner told them that when the life of a physician whose life was “thus well spent…” came to an end, he would feel “as if his mission had been properly accomplished, and that usefulness to others being its great and redeeming object, he had lived not for himself alone but for the comfort and happiness of those around him.” “With the time appropriated to his practice, to his studies, and to his notes, no physician can devote much to the ordinary pleasures and pursuits of life.”[9]
Civil War Surgeons’ medical education was severely limited by the concept that disease was caused by “bad air.” If only physicians could have theorized that particles were causative agents, they might have been able to wash them off, sweep them away, trap their carriers with netting, or poison them with chemicals. There was, however, no effective intervention with air being posited as the etiology of illness. Once disease affected their patients, physicians sought to correct a mal-distribution of the four humors―yellow bile, black bile, blood and lymph (a milky-colored liquid) ― they believed to occur in illnesses. The concept that all sickness was caused by four liquids of different colors called humors dates at least to the time of Hippocrates, 400 BC. These humors were thought to be in balance in bodies of healthy people. When they were out of balance, whether from ingested materials or arising within the body, disease occurred. Removal of liquids of many types from ill humans followed logically from this ancient theory. Amazingly, this humoral theory of disease was unquestioned for more than 2000 years, persisting until late in the 19th Century.
Not surprisingly, then, many treatments during the Civil War involved removal of fluids from the body. The sheer variety and number of substances administered boggles the mind, as we shall see. Agents and the sites they evacuated or the fluids they removed are shown in Table 3, with examples of each.
Table 3 Agents That Remove Bodily Substances[10]
The surgeons also administered stimulants, sedatives, tonics, and what they referred to as alteratives. The last group was believed to alter the course of a disease without loss of any fluid from the body, examples being mercury, iodine, and arsenic. Much mention is made of the widespread use of mercury during the War. Given by mouth in large doses, mercury (mercurous chloride only; the other form, mercuric chloride, is extremely toxic, causing blistering and shedding of the lining of the mouth, stomach, bowels, and death) acts as a cathartic. Used in small doses, however, it is slowly absorbed into the body. There are more than 400 cases in The Medical and Surgical History of the War of the Rebellion (1861–1865), in which mercury was prescribed for ill soldiers. Apart from using it as a laxative, surprisingly, surgeons caring for these men did not administer mercury randomly, but for a highly-selected group of diseases. They obeyed the standard of care for their time that was based on published guidelines and a detailed rationale for this treatment. The five conditions for which mercury was used were dysentery or diarrhea, typhoid fever, malaria, syphilis, and pneumonia. A case report of pneumonia follows, allowing us to examine how sick the soldier was, what treatment he received and the outcome of his illness. For treatment of the other four conditions the reader is referred to the Essential Civil War Curriculum of November 2012, entitled Disease in the Civil War.[11]
Case 3. —“A violent case in a dissipated subject. The patient stated that the day before he had a chill which was followed by fever and cough, with much pain in the side, so severe that he could scarcely breathe and did not sleep any during the night. He had violent cough with the characteristic rusty sputa [material brought up by coughing had the color of rust]; severe pain in the left side; great dyspnoea [difficulty breathing]; high fever; intense headache; pulse full, strong and frequent; skin hot and dry; face livid and anxious; respiration hurried; bowels constipated and urine scanty.
“1st day: Gave…mercurous chloride…and applied a blister over the seat of pain [an irritating substance placed on the skin caused a blister filled with fluid; the fluid thus produced was presumed to contain the noxious agent that caused the chest pain, drawing it out of the body]. 2d: Bowels well opened; the blister relieved the severe pain in the side; other symptoms unaltered. Gave brandy, eight ounces, morning, noon and night, with good nourishment. 3d: Very restless and sleepless during the night; symptoms unchanged. Gave twenty grains of sulphate of quinia [quinine, used here as a tonic, not for malaria], with half a grain of tartar emetic [antimony potassium tartrate, to induce vomiting], morning and evening; continued brandy and beef-tea. 4th: All the symptoms much improved; fever subsiding; pulse soft; skin moist; breathing easier; sputa mingled with less blood; secretion of urine copious. Diminished the quinia and tartar emetic by one-half; continued brandy and beef-tea. From this day complete convalescence was established and the patient soon recovered his strength—Surgeon Allen F. Peck, 1st N. M., Ft. Stanton, N.M., Dec. 31, 1862.” [12]
Other misconceptions about treatment during the War will now be discussed. One such is that anesthesia was rarely used. As Flannery documents in his detailed research, ether and chloroform were supplied to, and used widely by, military surgeons. Obviously these anesthetics were in short supply after Gettysburg, when on three consecutive days, some 50,000 casualties occurred; everything, including water and food, were also lacking then. During the successful Union blockade of southern ports late in the war, supplies were curtailed also. We know, moreover, that surgeons trained after 1848 had access to published information on how the two anesthetics were used. Amazingly, the American Medical Association (AMA), founded in 1847, started publishing the Transactions of the AMA only a few months later, in January of 1848. In the initial issue, that organization’s Committee on Anesthetic Agents published a history of the introduction of ether and chloroform into the practice of surgery, described the action of these agents on patients, reported the results of surgeons in the Jefferson Medical College and the University of Pennsylvania School of Medicine who used them, and urged the continued accumulation of information as their use widened. A final example is the popular misconception that amputations were done with abandon during the War. With the horrific injuries of soft tissue and bone inflicted by minié balls, gangrene with subsequent death of the soldier was assured in most. If anything, more surgery should have been performed. Numerous journals by surgeons contain a recurring refrain: if only they had amputated an injured limb sooner, this young man would not have died.[13]
Poor communication played a major role in the inadequate delivery of medical care during the Civil War. The record is full of examples of failure to implement proven new treatments of the sick and wounded. One critical discovery occurred a century before the Civil War. James Lind’s successful prevention and treatment of scurvy in 1753 went unheeded until 1785, when the British Navy finally adopted the use of citrus fruits on long voyages (This is, by the way, the origin of their sailors being called “limeys”.)[14]
Pierre Louis’ 1835 discovery that blood-letting had no benefit in several diseases was ignored well into the 19th Century. Perhaps its publication in French instead of English interfered with its dissemination to the United States. Despite Friedrich Wöhler’s publication in 1828 disproving the notion that a “life force” was needed to direct the functions of the body this concept of “vitalism” persisted into the 1870s. One reason why Wöhler’s seminal contributions might not have been disseminated more widely was that his paper was published in German, and his textbook on organic chemistry in French, Dutch, Danish, and Swedish, but not in English. The reason this example is so important is that it ignored the critical importance of biochemistry in understanding how the human body works. Not until Claude Bernard’s experiments were published in 1865, showing that physical and chemical reactions alone permitted all the body’s functions to occur and did not require any mysterious invisible vital force to do so, did knowledge of health and disease rapidly advance.[15]
Another tragic example was the independent publication by Oliver Wendell Holmes, Sr., in 1843 and Ignaz Philipp Semmelweis in 1847 that fatal infections were caused by doctors who did not wash their hands between examinations of patients. Holmes’ paper was in an obscure publication, and Semmelweis’ appeared in a German publication. There were medical journals at the time, but cases relating to war were scant. International medical conferences that continue to inform physicians and other scientists today did not begin until 1867. [16]
In contrast to these examples, effective prevention of smallpox, a virulent and often fatal disease was well understood by Civil War surgeons. So terrifying was smallpox that soldiers in both armies who developed it were isolated from any other troops, and their equipment, clothing, and anything else they had touched were burned or otherwise destroyed. The irony and the tragedy is that prevention had been known in England and Europe at least since the 1700s. Bayne-Jones reports that “inoculation against smallpox (the insertion into a normal individual, by scarification or puncture, of material from a fresh lesion [scab or blister] of smallpox, with the intention to produce a mild attack of the disease)…was applied in the British Army…before the start of the American Revolutionary War”. “By the time of the [American] Revolution, inoculation was practiced on general preventive grounds in the Colonies as it was in England.”
The medical term for conveying immunity using smallpox virus is variolation.[17]
Another safer way of preventing smallpox was discovered in 1798 by Edward Jenner, M.D. He discovered that shallow needling of scabs from milkmaids with cowpox (a non-fatal relative of smallpox) into the skin of persons never exposed to smallpox rendered them immune to this dreaded disease. Although Jenner’s patients with cowpox became ill, none of them died. In the same issue of The Vaccine Inquirer it is stated that in the United States vaccination with cowpox began in Maryland in 1801 with material from Jenner received eventually by Thomas Jefferson. The medical term for immunizing with cowpox virus is vaccination (vaccinus Latin word for cow). Inoculation refers to immunization with either virus.[18]
Studies published in 1822 documented the efficacy of universal vaccination in Europe. In the 12 years preceding vaccination in Denmark, there were 5,500 deaths from
smallpox in Copenhagen alone. In 1805 not one death occurred in the entire country. In Prussia in 1817 deaths from smallpox were reduced from 1 in 7 to 1 in 104. Sadly, during the Civil War at least 12,236 white Union troops developed smallpox (4,717 deaths), as did 6,716 colored troops (2,341 deaths). These numbers do not include soldiers cared for in either general or smallpox hospitals. Except for the Union Departments of the Northwest, of New Mexico, and of the Division of the Pacific, smallpox was present in every department during each year of the war. Among Confederate prisoners, 9,830 cases were reported with 2,624 dying of the disease.[19]
Why did thousands of soldiers develop smallpox, when prophylaxis against smallpox was proven effective and was practiced in civilian populations since the turn of the nineteenth century? Possible reasons include the following. Although the Union Army regulations required every man to be vaccinated, only a “few of the State military authorities succeeded in fulfilling this requirement. For many years before the war there had been no systematic vaccination in the [civilian] communities. Many of the volunteer troops had never been vaccinated [either].” When an epidemic of smallpox threatened the 1st, 6th, 9th and 27th Tennessee regiments just before the Battle of Missionary Ridge, Lieutenant William M. Cunningham of the 9th Tennessee was inoculated “with the virus of the smallpox and from the vaccine matter taken from his arm the whole brigade was vaccinated.” Many other men tried vaccinating themselves with scabs from fellow soldiers and developed what appeared to be syphilis. Since syphilis is also called great pox, it is easy to imagine non-medical troops confusing the two rashes and using the wrong one for self- inoculation. Syphilis-like rashes were reported even when soldiers were vaccinated by a surgeon with either officially-sanctioned crusts or those of a patient with smallpox.[20]
In the North, material for smallpox immunization was supplied by medical dispensaries in the form of crusts (scabs) obtained only from infants infected with the disease. Crusts collected on the twelfth to thirteenth day from cattle with naturally-occurring cowpox were also supplied to the Union Army to confer immunity against smallpox. Fear of spreading or acquiring syphilis, or of developing an abscess or even sepsis, made some surgeons and many soldiers hesitant to carry out orders to vaccinate.[21]
At least seven advances comprise the medical legacy of the Civil War. The three that directly improved care of the soldiers include triage of cases, an efficient ambulance system and invention of mobile army hospitals.
Triage prioritized the care of seriously wounded men needing immediate care (control of bleeding and probably surgery) at the edge of the battlefield over those too critical to be saved (given comfort and pain-relieving measures), and those whose injuries could be addressed at a later time. This innovation by US Surgeon Jonathan Letterman initiated the rapid removal of wounded soldiers from the battlefield.
A superb ambulance system, established by Letterman in 1862, further enhanced fast evacuation of wounded. He replaced command over ambulances by the quartermaster with that of the medical department. Consequently, soldiers, not random luggage or non-medical equipment, were transported quickly to field hospitals.
Mobile Army Hospitals organized by CS Surgeon Samuel Stout, Medical Director of Hospitals for the Confederate Army of Tennessee, allowed the safe relocation of ill and wounded men as battles occurred nearer them. This need arose as Stout had to move his patients deeper into the south ahead of invading Union armies.
The four remaining legacies did not directly affect patient care, but did so by expediting the availability of medical advances and information to physicians who adopted them into their medical practices. The Army Medical Museum founded in 1862 consisted of thousands of specimens collected, preserved and sent by Union surgeons to Washington, D.C. from surgeries as well as photographs and woodcuts of medical conditions. Renamed the National Museum of Health and Medicine in 1989, this superb research and historical source exists today.
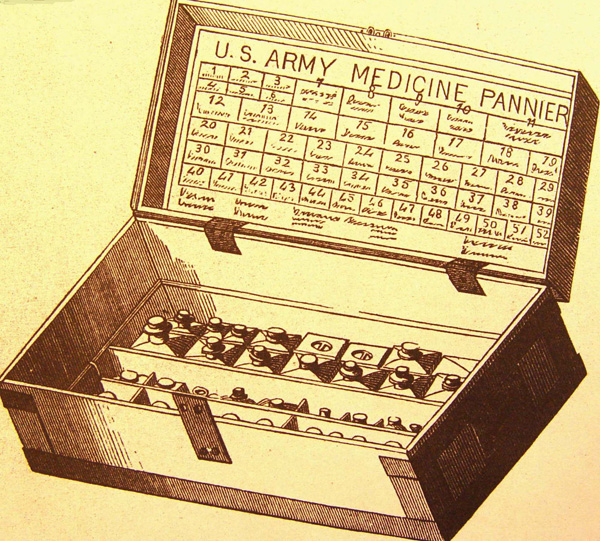
The Medical and Surgical History of the War of the Rebellion (1861-1865), published between 1870 and 1888 by the Government Printing Office and funded by Congress, continues to be a spectacular source of medical information, with thousands of case reports; illustrations of hospitals, tents, ambulances, panniers containing supplies carried by surgeons into the battlefield; essays by surgeons during and after battles; and reviews of journals and textbooks of the time.
The Index Medicus that began publication in 1879 contained scientific and other medical articles listed by subject and by author. Many physicians have used this work as the definitive source for advances in patient care and laboratory research for most of their professional lives. Renamed PUBMED in 2005, it now serves as the premier digital source of such information to a new generation of physicians and other scientists.
Finally The Library of the Office of the Surgeon General of the U.S. Army was founded in 1879, providing access to books and journals of the period. Renamed the National Library of Medicine in 1956, it is the world’s largest medical library and is now in Bethesda, Maryland.
Many physicians in the War did not survive into the 1880s and 1890s, but those who did saw the birth and development of the germ theory of disease—no more “bad air” causing infectious diseases, but living, breeding particulates that could be controlled initially in some measure by hand-washing, mosquito and fly control, antisepsis with noxious substances like phenol, and wearing masks or coughing into handkerchiefs to prevent droplet-borne diseases. The most grateful patients and gratified doctors, however, would be the ones who witnessed the first effective treatment of infected soldiers, using Salvarsan for syphilis in 1909, sulfa for many infections in 1935, and penicillin in 1943 for abscesses, “strep throat,” gonorrhea, and pneumonia. Sadly, using the limited knowledge and interventions available to them, surgeons in the Civil War saw more than 400,000 of their patients perish of diseases that can be treated or cured today. Lest we forget their heroic and dedicated efforts on behalf of their men, their splendid bequest to us, the monumental Medical and Surgical History of the War of the Rebellion (1861–1865), humbles us into respectful remembrance.
- [1] . Robert G. Slawson, “Medical Training in the United States Prior to the Civil War,” Journal of Evidence-Based Complementary & Alternative Medicine, 17 no.1 (January 2012), 11-27.
- [2] G.E. Dammann, Pictorial Encyclopedia of Civil War Medical Instruments and Equipment (Missoula, MT: Pictorial Histories Publishing, 1997) vol. 2. for school 1 in Table 1 and Slawson, Medical Training, for schools 2-29 in Table 1.
- [3] Slawson, Medical Training, for schools 1-13, 17-19, 21-23 in Table 2 and Dammann, Pictorial Encyclopedia, for schools 14-16 and 20 in Table 2.
- [4] Abraham Flexner, Medical Education in the United States and Canada Bulletin Number Four (Boston: D.B. Updike, Merrymount Press, 1910). Abraham Flexner was commissioned by the Carnegie Foundation for the Advancement of Teaching to examine all medical schools in the United States and Canada, recording requirements for admission, curricula, qualifications of professors, laboratory facilities, and availability of patients to students that permitted them to learn directly about patient care. His ground-breaking report changed medical education forever in both countries.
- [5] Catalogue of the Trustees, Officers & Students of the University of Pennsylvania, Session 1850–51. (Philadelphia: L.R. Bailey, Printer, 1851), 36.
- [6] G.B. Wood, Introductory to the Course of Lectures on the Theory and Practice of Medicine, in the University of Pennsylvania, Delivered October 11, 1850 (Philadelphia: Merrihew and Thompson, Printers; 1850), 8-9.
- [7] Ibid., 10; Ibid., 18.
- [8] Samuel Jackson, An introductory lecture, preliminary to a course on the Institutes of Medicine, delivered on the 9thof October, 1850, before the class of the University of Pennsylvania (Philadelphia: Journeymen Printers’ Office, 1850),18.
- [9] W.E. Horner, Medical Commencement of the University of Pennsylvania held on Saturday, April 5, 1851: with a Valedictory by W. E. Horner, M.D., Professor of Anatomy. (Philadelphia: L.R. Bailey, Printer, 1851), 15, 18.
- [10] B.B. Dorwart, Carson’s Materia Medica of 1851: An Annotation (Bala Cynwyd, PA: WVD Press, 2003), 11–76.
- [11] Joseph Woodward et al, The Medical and Surgical History of the War of the Rebellion 1861-65 (Washington D.C.: Government Printing Office, 1870-1888); (hereafter cited as MSHWR).
- [12] Ibid., 6:752.
- [13] M.A. Flannery, Civil War Pharmacy: A History of Drugs, Drug Supply and Provision, and Therapeutics for the Union and Confederacy ( New York: Pharmaceutical Products Press, 2004 ); Transactions of the American Medical Association 1 (1848): 176, 214, 220–1.
- [14] C.P Stewart and D. Guthrie, eds. Lind’s Treatise on Scurvy. Reprint of the first edition of James Lind of 1753 (Edinburgh: Edinburgh University Press, 1953), 145–148.
- [15] F. Wöhler, Annalen der Physik und Chemie, 2nd series 12; 1828), 252–6
- [16] Oliver Wendell Holmes, Sr. “The Contagiousness of Puerperal Fever. Read before the Boston Society for Medical Improvement and published at the request of the Society”, New England Quarterly Journal of Medicine and Surgery, 1843, 1-28.
- [17] S. Bayne-Jones, The Evolution of Preventive Medicine in the U.S. Army, 1607–1939 (Washington: U.S. Government Printing Office, 1968), 17, 21.
- [18] E. Jenner E., “An Inquiry Into the Causes and Effects of the Varioloe Vaccinoe, A Disease Discovered in Some of the Western Counties of England—Particularly Gloucestershire, and Known by the Name Of The Cowpox, London 1798”, The Vaccine Inquirer, Vol. I. Baltimore: John D. Toy; 1822: 1–15; Ibid., 16-23.
- [19] Ibid., 95; Ibid., 96; James I. Robertson Jr., The Medical and Surgical History of the Civil War (Wilmington, NC: Broadfoot, 1990), 1:637 (hereafter cited as MSHCW); Ibid., 1:710; Ibid., 6:625;Ibid., 6:627.
- [20] Ibid., 626; .” R.C. Forrester, Glory and Tears: Obion County, Tennessee 1860–1870. (Union City, TN: H.A. Lanzer, 1966), 178; MSHCW 6: 636; Ibid., 627.
- [21] Ibid., 634.
If you can read only one book:
Burton, Brian K. Extraordinary Circumstances: The Seven Days Battles. Bloomington: Indiana University Press, 2001.
Books:
Boland, F.K. The First Anesthetic: The Story of Crawford Long. Athens: University of Georgia Press, 1950.
Dammann, G.E. Pictorial Encyclopedia of Civil War Medical Instruments and Equipment. Missoula, MT: Pictorial Histories Publishing, 1997, 2:29-31.
Dorwart, B.B. Carson’s Materia Medica of 1851: An Annotation. Bala Cynwyd, PA: WVD Press, 2003.
Duffy, J. The Sanitarians: A History of American Public Health. Champaign: University of Illinois Press, 1990.
Flannery, M.A. Civil War Pharmacy: A History of Drugs, Drug Supply and Provision, and Therapeutics for the Union and Confederacy. New York: Pharmaceutical Products Press, 2004.
Hasegawa, G.R. and F.T. Hambrecht. “The Confederate Medical Laboratories” Southern Medical Journal, 96:1221 (2003).
Schwartz, Gerald, ed. A Woman Doctor’s Civil War, Esther Hill Hawks’ Diary. Columbia: University of South Carolina Press, 1984.
Slawson, R.G. Prologue to Change: African Americans in Medicine in the Civil War Era. Frederick, MD: National Museum of Civil War Medicine Press, 2006.
———. “Medical Training in the United States Prior to the Civil War,” Journal of Evidence-Based Complementary & Alternative Medicine, 17 no.1 (January 2012).
Organizations:
No organizations listed.
Web Resources:
The National Museum of Civil War Medicine (NMCWM) is the only non-governmental museum devoted to Civil War Medicine in the United States. The museum contains exhibits, vintage tents and ambulances. It holds an annual meeting with peer-reviewed abstracts and it operates the NMCWM Press. 48 East Patrick Street Frederick, MD 21705 (301) 695-1864. 10:00-5:00 M-S 11:00-5:00 Sun.
The specific goal of The Society of Civil War Surgeons is to promote, in both members as well as the general public, a deep and abiding appreciation for rich medical heritage of the American Civil War. Peer reviewed papers are published quarterly and an annual meeting is held with peer reviewed abstracts.
Other Sources:
No other sources listed.